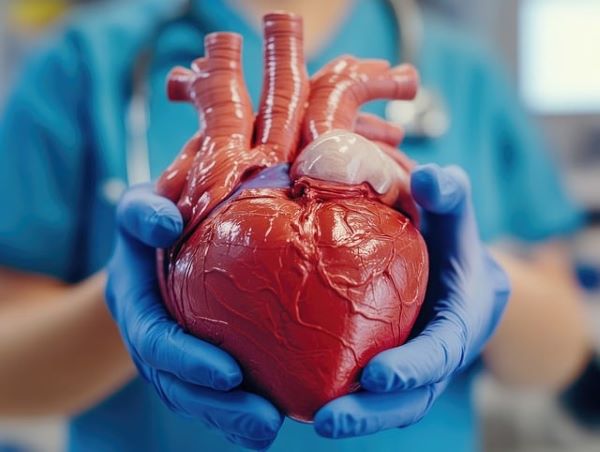
A Ventricular Septal Defect (VSD) is one of the most common congenital heart defects, characterized by a hole in the wall (septum) that separates the heart’s lower chambers (ventricles). This defect allows oxygen-rich blood from the left ventricle to mix with oxygen-poor blood from the right ventricle, putting extra strain on the heart and lungs. VSDs vary in size, with larger defects potentially leading to serious complications like heart failure, while smaller ones may close on their own without requiring medical intervention. (Source)
What is a Ventricular Septal Defect?
A VSD occurs when there is an abnormal opening in the septum dividing the two ventricles of the heart. In a normal heart, the septum acts as a barrier between the oxygen-rich blood in the left ventricle and the oxygen-poor blood in the right ventricle. However, in the presence of a VSD, blood can pass from the left side of the heart to the right side, causing the heart to pump extra blood to the lungs. This increases the workload on the heart and can lead to symptoms such as fatigue, rapid breathing, and poor growth in infants.
VSDs can occur in different parts of the septum and are categorized based on their location and size:
- Perimembranous VSD: Occurs in the upper part of the ventricular septum near the heart valves.
- Muscular VSD: Located in the lower, muscular part of the septum.
- Inlet VSD: Found near the tricuspid and mitral valves.
- Outlet VSD: Near the pulmonary and aortic valves.
VSD is often diagnosed in infancy or early childhood, but it can sometimes remain undetected until later in life. (Source)
Also, read: Now Know All about Cleft Palate: Cause, Symptoms, Diagnosis, Treatment
How is VSD Caused?
Ventricular septal defects develop during the early stages of fetal heart formation. The heart starts as a simple tube and gradually forms four chambers (two atria and two ventricles) as it grows. If something disrupts this process, the septum between the ventricles may not form completely, leading to a VSD.
While the exact cause of VSD is not always known, several factors contribute to its development:
- Genetic Factors: Some VSDs are associated with genetic syndromes, such as Down syndrome, where multiple congenital anomalies occur due to a chromosomal abnormality. Mutations in genes that regulate heart development can also lead to the condition.
- Environmental Factors: Certain environmental factors during pregnancy, such as maternal diabetes, smoking, alcohol consumption, or medication use (like anti-seizure drugs), can increase the risk of VSD. (Source)
History and Science of VSD
VSD has been recognized as a congenital heart defect for centuries, but the understanding of its pathology and treatment has significantly advanced in the modern medical era. In the 19th century, early descriptions of VSDs were made by medical pioneers studying heart anatomy and congenital anomalies.
- The first successful surgical repair of a VSD occurred in the 1950s, thanks to advances in cardiopulmonary bypass techniques that allowed surgeons to stop the heart and operate inside it.
- By the 1970s, more refined surgical techniques and innovations, such as the use of synthetic patches to close VSDs, became standard in pediatric heart surgery.
Advances in prenatal imaging, such as fetal echocardiography, now allow doctors to diagnose VSDs before birth, offering the possibility of early intervention. (Source)
Risk Factors for VSD
Several risk factors can increase the likelihood of a VSD developing in a fetus:
- Family History: If a parent or sibling has had a congenital heart defect, there is an increased risk of VSD occurring in future pregnancies.
- Genetic Disorders: Certain genetic conditions, such as Down syndrome and other chromosomal abnormalities, are associated with a higher incidence of VSD.
- Maternal Health: Maternal illnesses, including diabetes and rubella infection during pregnancy, can contribute to the development of VSD.
- Lifestyle Factors: Smoking, excessive alcohol consumption, and use of certain drugs during pregnancy can increase the risk of heart defects.
- Advanced Maternal Age: Women who become pregnant later in life may be at a higher risk of having a baby with congenital heart defects, including VSD. (Source)
Treatment for VSD
The treatment for a ventricular septal defect depends on the size of the hole, the severity of the symptoms, and the overall health of the child. Many small VSDs close on their own during the first few years of life and may not require treatment.
- Observation: In mild cases, where the defect is small, doctors may recommend regular monitoring to see if the VSD closes on its own. During this time, the child’s growth, breathing, and heart function will be carefully tracked.
- Medications: For moderate to severe VSDs that cause symptoms like heart failure, medications may be prescribed to help the heart function more effectively. These include:
- Diuretics: To reduce the amount of fluid in the lungs and ease breathing.
- ACE inhibitors: To lower blood pressure and reduce the workload on the heart.
- Beta-blockers: To slow the heart rate and improve heart function.
- Surgical Repair: In cases where the VSD is large or causing complications, surgery may be necessary to close the hole. The procedure involves patching the opening with a synthetic material or sewing the tissue together to create a solid barrier between the ventricles.
- Surgery is usually performed through open-heart surgery, but in some cases, minimally invasive catheter-based techniques can be used.
- Cardiac Catheterization: Some small VSDs can be closed using a catheter-based procedure. A thin tube (catheter) is inserted through a blood vessel in the groin and guided to the heart, where a device is used to plug the hole. (Source)
Can VSD Be Prevented?
There is no surefire way to prevent congenital heart defects, including VSD, but certain steps can reduce the risk:
- Prenatal Care: Regular check-ups during pregnancy allow for early detection of problems and management of risk factors like diabetes and high blood pressure.
- Healthy Lifestyle Choices: Avoiding alcohol, smoking, and harmful medications during pregnancy can decrease the risk of birth defects.
- Genetic Counseling: If there is a family history of congenital heart defects or genetic disorders, seeking genetic counseling before pregnancy can help assess risks and plan for early diagnosis.
Is VSD Hereditary?
VSD can be hereditary, as genetic factors play a role in some cases. Parents who have had a child with VSD or have a family history of congenital heart defects are at higher risk of having another child with the condition. Genetic conditions like Down syndrome are also linked to an increased risk of VSD. (Source)
Can VSD Be Cured?
Yes, VSD can be cured, especially with early diagnosis and appropriate treatment. Many small VSDs close on their own without intervention, while larger defects often require surgery to repair. After successful treatment, most children lead normal, healthy lives, though ongoing follow-up may be necessary to monitor heart function.
Also, watch web stories: 7 Facts You Need to Know About Neuroblastoma
Conclusion
Ventricular septal defect (VSD) is a common congenital heart defect caused by an incomplete formation of the septum between the heart’s ventricles during fetal development. While the exact causes of VSD are not fully understood, genetic and environmental factors contribute to its occurrence. The defect can vary in severity, with treatment options ranging from observation to surgery. Advances in surgical techniques and medical care mean that VSD is highly treatable, and with proper care, most children can expect a good quality of life.