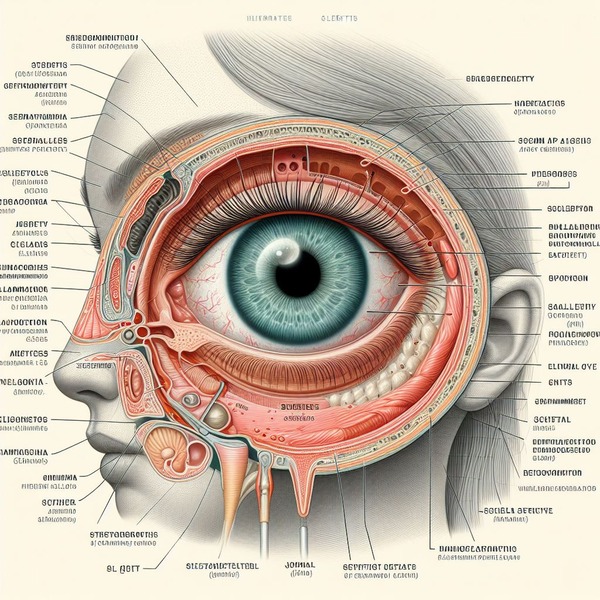
What is Scleritis?
It is the eye’s protective outer coat, as well as the white component of the eye. It is linked to muscles which help in eye movement. The sclera covers around 83 percent of the eye surface. It is a condition in which the sclera becomes inflamed and red. It can be excruciatingly uncomfortable. Scleritis is thought to be caused by the body’s immune system responding. The location of the inflammation determines the sort of scleritis you have. The illness causes considerable discomfort in the majority of patients, but there are exceptions. Source
It must be treated with medication as soon as possible to prevent it from progressing. Serious cases that go untreated might result in partial or whole visual loss.
Also, read Complete Information about Cataracts: Causes, Symptoms and Treatment
Types of Scleritis
It is classified into two types: anterior (relating to the front of your sclera) and posterior (referring to the back of your sclera). Scleritis, both anterior and posterior, can be diffuse, nodular, or necrotizing. Source
- Diffuse scleritis: Diffuse is spread across your sclera. It is the most prevalent.
- Nodular scleritis: It is a type of scleritis that is confined to one area of the sclera. The bulge (nodule) is frequently visible.
- Necrotizing scleritis: This most severe form of it. It can harm ocular tissue and potentially result in the loss of a whole eye. Scleromalacia perforans is a kind of necrotizing scleritis. Although it is not unpleasant, it can result in perforations (holes). This kind accounts for 4% of all scleritis cases.
Symptoms
The signs and symptoms of it include:
- Redness and swelling of your sclera.
- Pain and soreness in your eye, which is often severe enough to keep you up at night. It can spread to other parts of your face as well.
- Watering (tearing) eyes.
- Light sensitivity (photophobia).
Causes
It can have no recognized cause. This is referred to by doctors as “idiopathic.” In many other circumstances, scleritis might develop as a result of another medical condition, such as an autoimmune disease. Scleritis can also be linked to:
- Infections – Infectious is caused by some illnesses. These can be bacterial, fungal, or viral. Fungal infections typically have a worse prognosis than bacterial or viral infections. Scleritis (Lyme scleritis) can be caused by Lyme disease.
- Trauma or injury to your eye, including surgical procedures – This type of injury frequently causes infected scleritis. One example is a condition known as surgically induced necrotizing scleritis (SINS).
- Medications used to treat or prevent bone disorder – These types of medications such as bisphosphonates, are known to trigger inflammatory ocular reactions.
Risk factors
Scleritis may occur at any age. It is more likely to develop in women than in men. There is no particular race or region of the world where this illness is more prevalent.
You are more likely to acquire scleritis if you have:
- Wegener’s disease (Wegener’s granulomatosis), is an uncommon disorder that includes blood vessel inflammation. Source
- Rheumatoid arthritis (RA) is an autoimmune disorder defined by joint inflammation. Source
- Inflammatory bowel disease (IBD) is identified by digestive symptoms caused by bowel inflammation. Source
- Sjogren’s syndrome is an immunological condition causing dry eyes and mouth. Source
- Lupus is an immune disorder that causes skin inflammation. Source
- Eye infections (which may or may not be related to autoimmune illness) damage to eye tissues from an accident
Diagnosis
Your doctor may be likely to diagnose scleritis by doing an eye exam, which may involve a slit lamp exam. Your doctor may inquire about your history of systemic illnesses, such as RA, Wegener’s granulomatosis, or IBD. They may also inquire as to whether you have a history of eye injuries or surgery.
The tests listed below can assist your doctor in making a diagnosis:
Ultrasonography is used to detect changes in or around the sclera.
Complete blood count is performed to look for symptoms of infection and immune system activity
A sclera biopsy, which includes extracting tissue from the sclera to be viewed under a microscope
Treatment
It’s treatment focuses on reducing inflammation before it causes permanent damage. The treatment is delivered in a step-by-step fashion. If the first pharmaceutical step fails, the second is used.
The following medications are used to treat scleritis: Source
- When treating nodular anterior scleritis, nonsteroidal anti-inflammatory medications (NSAIDs) are most frequently used. Pain from scleritis can also be lessened by reducing inflammation.
- If NSAIDs are ineffective in reducing inflammation, corticosteroid medications (like prednisone) may be administered.
- For posterior scleritis, oral glucocorticoids are the recommended treatment.
- Oral glucocorticoids combined with immunosuppressive medications are the recommended treatment for necrotizing scleritis, the most severe kind.
- It’s infections can be prevented or treated with antibiotics.
- Antifungal drugs are frequently prescribed for infections caused by Sjogren’s syndrome.
Prevention
It is usually not preventable. However, you may look after your eyes well. If you use the proper eye protection at work or when playing certain contact sports, you can lower your chance of causing damage to your eyes. If you must touch your eyes, make sure your hands are clean to lower your chance of developing an eye infection. If you wear contacts, be careful to clean those as well.
Also, read Complete Guide on Dry Eye: Causes, Symptoms and Treatment