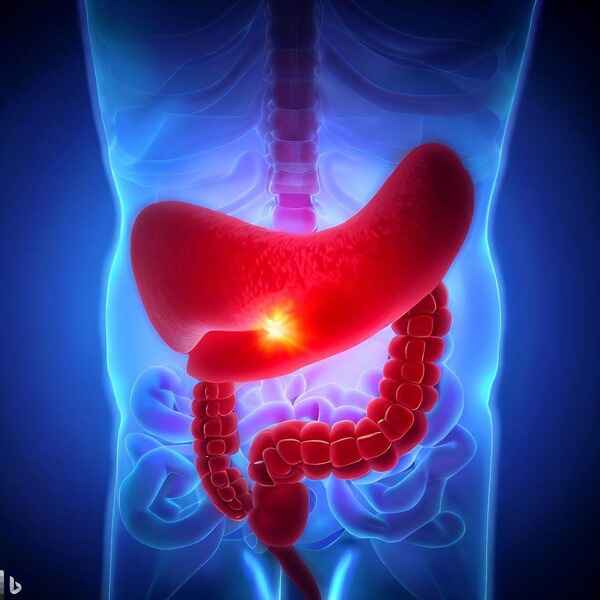
What is Pancreatitis?
Pancreatitis is pancreatic inflammation (swelling). The pancreas is a gland located near the stomach and liver. It produces digestive fluids and enzymes. These aid in the absorption and digestion of meals.
Pancreatitis develops when pancreatic enzymes begin to break down pancreatic tissues. This can result in edema, hemorrhage, and pancreatic damage. Pancreatitis can be caused by gallstones, excessive alcohol consumption, and certain medications.
Pancreatitis is classified into two types: acute and chronic. “Pancreatitis” is sometimes used alternately with “acute pancreatitis,” because this form of the disease, which occurs rapidly and lasts a short period of time, is the most common.
Also, Read Understanding Diabetes: What is Diabetes? Types, Causes, Symptoms, Management
Causes
The top two causes of pancreatitis include:
- Gallstones – Through the same aperture as your pancreatic duct, your common bile duct dumps bile from your gallbladder into your gut. If a gallstone enters the common bile duct and becomes lodged at the junction, it might temporarily obstruct pancreatic juice discharge. This traps enzymes within your pancreas. As pressure builds up behind the obstruction, the enzymes inside your pancreas become activated and begin digesting the pancreas itself. This results in the inflammatory reaction associated with gallstone pancreatitis.
- Heavy drinking – Another apparent cause of pancreatitis is excessive alcohol consumption, though. The poisonous remnants of alcohol in your blood may produce an inflammatory response in your pancreas, or they may chemically activate the digestion enzymes within your pancreas. According to scientists, strong alcohol usage accounts for around half of all acute and chronic pancreatitis occurrences.
Together, these factors account for nearly 80% of pancreatitis cases.
Symptoms
The symptoms of each individual may differ. Symptoms could include:
- Severe abdominal discomfort that may move to your back or chest (may be worse after eating)
- Nausea
- Vomiting
- High heart rate
- Fever
- Upper belly swelling and soreness or tenderness
- Fluid accumulation in your abdomen
- Blood pressure has been reduced.
- Jaundice (yellowing of the skin and eyes).
Risk factors
The following conditions can lead to acute pancreatitis:
- Gallstones
- Alcoholism
- Multiple medications
- Hypertriglyceridemia (high triglyceride levels in the blood)
- Hyperparathyroidism, or hypercalcemia, is a condition where the parathyroid glands are overactive and cause excessive blood calcium levels.
- Pancreatic cancer
- Abdominal surgery
- Cystic fibrosis
- Infection
- Injury to the abdomen
- Obesity
- Trauma

Diagnosis
To determine if you have acute or chronic pancreatitis, your doctor will perform a physical examination, run blood tests, and ask for imaging tests. Your doctor may feel your stomach during the physical examination to see whether your muscles are stiff or your stomach is sore.
The blood test counts how much of two digestive enzymes are present in the pancreas; nevertheless, it cannot accurately identify pancreatitis. The levels of those enzymes increase with the start of acute pancreatitis and are frequently greater than three times normal. Other blood tests can check the white blood cell count and renal function.
The imaging exams mentioned below may also be prescribed by your doctor to look for inflammation, gallstones, and other changes:
- X-rays
- Ultrasounds
- Computerized tomography (CT) scans
- Endoscopic ultrasounds (EUS)
- Magnetic resonance cholangiopancreatography (MRCP)
Treatment
You may need to stay in the hospital for a few days if you have acute pancreatitis. There, you can get intravenous (IV) fluids, antibiotics, and pain medication. The majority of mild episodes of pancreatitis resolve with therapy and rest.
If your pancreatitis is severe, you may require additional therapy. Depending on the cause of the pancreatitis, this treatment could include:
- Removing the Gallbladder – Your gallbladder may need to be removed if you have gallstones.
- Other procedures – Your doctor might need to drain an abscess or pseudocyst if it is infected. If necessary, he or she can remove harmed tissue from your pancreas. They can perform additional procedures to address issues with the pancreatic and bile ducts.
If you have chronic pancreatitis, your treatment plan will assist in relieving pain, improving the function of your pancreas, and managing complications. It could include:
- A low-fat diet
- Pain reliever medication
- Insulin is used to treat high blood sugar levels.
- Enzyme tablets (pills that help with digestion)
If your body does not absorb nutrients efficiently, you may need to take vitamins. Someone with chronic pancreatitis may also require surgery. This might help in the relief of pressure or a blockage in a pancreatic duct. Surgery may also be performed to remove a damaged or infected pancreatic.
People with pancreatitis should not consume alcohol or smoke. Due to the harm caused by chronic pancreatitis, some people acquire diabetes or pancreatic cancer. These medical conditions require different therapies.

Diet
What you should eat
- Low-fat or fat-free milk and yogurt or dairy-free alternatives such as almond, soy, and rice milk
- Fruits and vegetables
- Grains
- Protein
Also, Read Dates Health Benefits: Nutritional Value and Uses
What you should not eat
- High-fat foods
- High-sugar foods and Refined carbohydrates
- Alcoholic beverages
Prevention
- Create a low-fat, healthy food plan with the help of your doctor.
- Stop drinking alcohol and give up smoking. Consult your doctor about quitting options.
- To stay hydrated, drink lots of water.
- Consult your doctor if chronic pancreatitis is contributing to your depression. Taking antidepressant medication or speaking with a counselor about how you’re feeling may be helpful.
- getting more sleep or working out.
- Take up some relaxing techniques to lower your tension.