This research article on Managing Chronic Kidney Disease published in HealthViews India is written by Rohan Bhadange, Anil Bhanudas Gaikwad – Professor, Department of Pharmacy, Birla Institute of Technology and Science, Pilani, Pilani Campus, Vidya Vihar, Pilani, Rajasthan 333031, India.
Abstract: The kidneys play important bodily functions such as the excretion of waste and excess water, regulation of electrolyte balance, regulation of blood pressure, and red blood cell production. Chronic kidney disease (CKD) slows down all mentioned functions in the body and usual symptoms include frothy urine, low urine output, nausea, loss of appetite, and tiredness, among others. CKD is a major health issue with rising cases day by day, leading to severe health concerns and deaths. The most common causes of CKD progression include high blood pressure, heart-related disease, diabetes, obesity, smoking, nephrotoxic medicines, and other kidney-related issues. The diagnosis of CKD in the early stage is important because most patients living with CKD, do not know whether they have CKD. The early diagnosis will help to control the disease severity in CKD patients. Its diagnosis involves blood, urine, imaging, and kidney sample tests. The therapeutic management of CKD involves blood pressure-relieving medications, fluid replenishers, medications to treat anemia, cholesterol-lowering drugs, and bone-protecting agents. Exercise, yoga, meditation, and dietary management along with therapeutic management often relieve CKD-related symptoms in patients. Currently, available therapies in the management of CKD are not fully effective and often lead to side effects. The use of licensed and existing medications (drug repurposing) is becoming more advantageous nowadays. Hence, researchers are dedicated to finding better treatment options in the management of CKD.
The kidneys
The human kidneys have two kidneys found behind the abdominal (back) area, on either side of the vertebral column, just below the rib cages. They are important organs that perform essential functions in the body. Its main function is to excrete waste from blood and excess water in the form of urine. The kidneys help regulate electrolyte and mineral levels, produce hormones for blood pressure regulation and red blood cell production, and keep bones strong. When they are damaged, waste builds up in the blood, leading to kidney-related issues [1].
The kidneys may perform abnormal functions in the presence of kidney-related diseases and may cause complications in the body, leading to death in severe cases. Various kidney-related diseases include acute kidney injury (AKI), chronic kidney disease (CKD), diabetic kidney disease (DKD), Polycystic kidney disease (PKD) and renal cell carcinoma (RCC), among others.
Also Read: What is Dialysis: Types, Process, Benefits and Diet for Patients Undergoing Dialysis
Chronic Kidney Disease
CKD is a type of kidney disease that lasts long and continues for more than three months and causes a slow decline in kidney function. Signs of kidney problems include protein in the urine, unusual urine test results, or issues found through scans or biopsies [2]. More than 800 million people worldwide suffer from CKD, with higher rates among older individuals, women, and those with diabetes and hypertension.
CKD has become a major global health concern, rising from the 36th to the 19th leading cause of years of life lost between 1990 and 2013 [3]. This can lead to the need for dialysis or a kidney transplant in severe kidney malfunctioning cases. As CKD cases continue to rise, finding new ways to diagnose and treat the disease is important. Current therapies in the management of CKD can help with symptoms but cannot fully cure the disease.
Moreover, the use of licensed and existing medications (drug repurposing) is becoming more advantageous nowadays. Since it cuts down on the time and expenses needed for the development of new drug candidates (medication), repurposing of drugs improves the quality of life of patients suffering from CKD. Therefore, drug repurposing can be a better approach to developing effective medications in the management of CKD. Hence, researchers are dedicated to finding better treatment options in the management of CKD [4, 5].
Stages of CKD
The stages of CKD range from stage 1 to stage 5, which are classified by how well the kidneys filter out the wastes from the body.
- Stage 1: a normal eGFR above 90 ml/min (with detected signs of kidney damage)
- Stage 2: a sightly reduces eGFR of 60 to 89ml/min
- Stage 3: stage 3a – an eGFR of 45 to 59ml/min; stage 3b – an eGFR of 30 to 44ml/min
- Stage 4: an eGFR of 15 to 29ml/min
- Stage 5: an eGFR below 15ml/min (almost all kidney functions have stopped) [6].
Signs and symptoms of CKD
Most people living with CKD, do not know whether they have CKD. This is because the symptoms of this disease are often silent and most people are diagnosed with this disease when it reaches to the last stage. Patients with CKD have the following signs and symptoms (Fig. 1),
- Frothy urine
- Low urine output
- Nausea
- Loss of appetite
- Tiredness
- Weight loss
- Dry/itchy skin
- Puffy eyes
- Swelling of hands, ankles, feet.
Causes of CKD
CKD can be caused by many factors, the most common factors responsible for CKD progression include (Fig. 1),
- High blood pressure
- Heart-related diseases
- Diabetes
- Obesity
- Smoking
- Use of medicines that are toxic to the kidneys (nephrotoxic medicines)
- Other kidney-related issues such as kidney stones, AKI, systemic lupus erythematosus, and renal artery stenosis, among others [7].
Also Read: Complete Details on Kidney Profile KFT Test: What Blood Tests Does It Cover?
Diagnosis of CKD
The doctor starts diagnosing CKD by asking about the medical history of the patient. Your doctor may ask, among other things, if you have observed changes in your urine color, if you have a history of high blood pressure, if you may have kidney diseases in your family, or have taken any medications that may affect kidney functions.
Doctors often ask patients about a few tests or procedures to diagnose and determine the diagnosis or the stage of CKD. Such tests include (Fig. 1),
- Blood tests: Blood creatinine and urea tests are often used to check kidney functions.
- Urine tests: Urine-creatinine ratio can be tested to diagnose the abnormalities in the patient’s urine.
- Imaging tests: Imaging tests, such as ultrasound scan, CT or MRI scan, can be used to assess the structure and size of the kidneys.
- Kidney sample test: In more severe cases, doctors often ask patients for a biopsy. A biopsy involves the insertion of a long needle into the kidneys, the collection of samples, and the sending of the samples to the pathological labs that may help to find the cause of the kidney disease [6, 8].
Management of Chronic Kidney Disease
- Therapeutic management for CKD: In therapeutic management, doctors often prescribe medications to relieve CKD-related symptoms. Such treatment options include (Fig. 1),
- Blood pressure relieving medications: In patients with CKD, high blood pressure may worsen over time. Doctors frequently recommend medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers to control blood pressure and safeguard kidney function.
- Fluid retention treatment (fluid replenishers): Patients with CKD may accumulate excess fluid, causing leg swelling and hypertension. Diuretic medications help remove excess fluid, maintain balance in the body and minimize the CKD-associated risk.
- Medications to treat anemia: Anemia is a frequent problem in CKD, making people feel weak and tired. The kidneys play a key role in producing erythropoietin, a hormone that helps create red blood cells to carry oxygen in the body. To manage anemia, erythropoietin supplements may be prescribed, often with iron, to increase red blood cell production, reducing the tiredness and weakness linked to anemia.
- Medications to lower cholesterol levels (cholesterol-lowering drugs): High levels of bad cholesterol are common in CKD and can contribute to the risk of developing heart diseases. Hence, medications like statins may be advised to manage cholesterol levels.
- Bone protecting agents: Calcium and vitamin D supplementation helps prevent bone weakness and fractures, while medications reduce phosphate levels in the blood, preventing calcium deposits that could harm blood vessels [9, 10].
Managing Chronic Kidney Disease: Home Remedies and Dietary Management
Along with therapeutic management, doctors ask patients to follow a diet plan that helps to support kidney functions (Fig. 1).
- Avoid high salt-containing food: A high salt-containing diet may worsen CKD complications; hence CKD patients should avoid food items with added salts, fast food, frozen meat, and snacks.
- Low protein diet: A high protein consumption can lead to CKD progression. Hence, dietary intake of high protein should be restricted to patients with CKD such as cheese, milk, eggs, and meats.
- Food with low potassium levels: Patients with CKD should avoid high potassium-containing food such as tomatoes, potatoes, bananas, oranges and spinach. Instead, patients may take a low-potassium diet such as grapes, strawberries, carrots, and apples, among others [11, 12].
- Exercise: Age and physical health decide the type of exercise that suits the patient the best. Patients should ask their doctor about exercise plans. Walking, jogging, yoga, meditation, swimming, and outdoor sports such as basketball, and tennis, may help to manage CKD-associated health issues that help to prevent CKD progression [13].
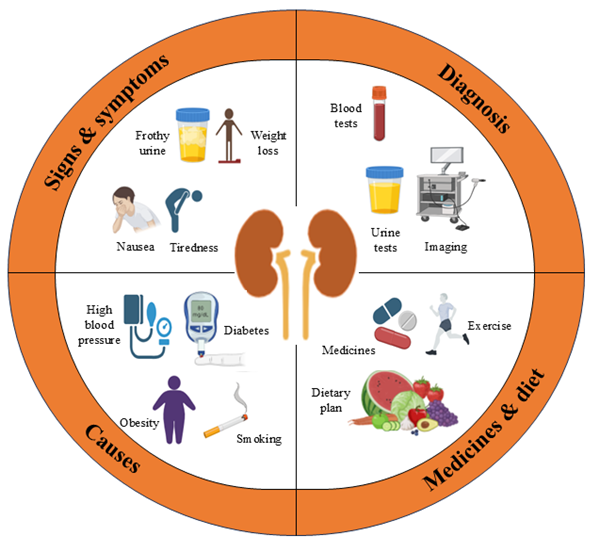
Fig. 1. Managing Chronic kidney disease: Signs & symptoms, causes, diagnosis and medicines & diet management
Summary
CKD affects millions of people worldwide, but early diagnosis and proper management can help slow its progression and improve patients’ quality of life. Current treatments focus on relieving symptoms and improving quality of life, but there is still no complete cure. Scientists are continuously working on new therapies to better manage the disease. Healthy lifestyle choices, such as a balanced diet and medication, play a crucial role in treatment. Regular screenings can help detect CKD early and prevent serious complications. Raising awareness about kidney health is important to reduce the global burden of CKD. With ongoing research and improved medical care, there is hope for a future with better treatment options in the management of CKD.
Acknowledgements
ABG sincerely acknowledges the Anusandhan National Research Foundation (ANRF)- Empowerment and Equity Opportunities for Excellence in Science (EMEQ), Department of Science and Technology, Government of India [EEQ/2023/000014] for their financial support.
This research article on Managing Chronic Kidney Disease published in HealthViews India is written by Rohan Bhadange, Anil Bhanudas Gaikwad – Professor, Department of Pharmacy, Birla Institute of Technology and Science, Pilani, Pilani Campus, Vidya Vihar, Pilani, Rajasthan 333031, India. You can contact the author at: anil.gaikwad@pilani.bits-pilani.ac.in
References:
1. Gilbert, S.F. and D.E. Weiner, National kidney foundation primer on kidney diseases, E-Book. 2022: Elsevier Health Sciences.
2. Vaidya, S.R. and N.R. Aeddula, Chronic kidney disease, in StatPearls [Internet]. 2024, StatPearls Publishing.
3. Kovesdy, C.P., Epidemiology of chronic kidney disease: an update 2022. Kidney international supplements, 2022. 12(1): p. 7-11.
4. Bhadange, R. and A.B. Gaikwad, Repurposing the familiar: Future treatment options against chronic kidney disease. Journal of Pharmacy and Pharmacology, 2025: p. rgaf002.
5. Panchapakesan, U. and C. Pollock, Drug repurposing in kidney disease. Kidney international, 2018. 94(1): p. 40-48.
6. Romagnani, P., et al., Chronic kidney disease. Nature reviews Disease primers, 2017. 3(1): p. 1-24.
7. Ammirati, A.L., Chronic kidney disease. Revista da Associação Médica Brasileira, 2020. 66(Suppl 1): p. s03-s09.
8. jp, J.S.o.N.o.j.o., Essential points from evidence-based clinical practice guideline for chronic kidney disease 2023. Clinical and Experimental Nephrology, 2024. 28(6): p. 473-495.
9. Knicely, D.H. and S. Thavarajah, Chronic Kidney Disease Management Programs and Patient Education, in Management of Chronic Kidney Disease: A Clinician’s Guide. 2023, Springer. p. 525-534.
10. Kushner, P., et al., Early identification and management of chronic kidney disease: A narrative review of the crucial role of primary care practitioners. Advances in Therapy, 2024. 41(10): p. 3757-3770.
11. Yan, M.-T., C.-T. Chao, and S.-H. Lin, Chronic kidney disease: strategies to retard progression. International journal of molecular sciences, 2021. 22(18): p. 10084.
12. Levin, A., et al., Executive summary of the KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease: known knowns and known unknowns. Kidney international, 2024. 105(4): p. 684-701.
13. Mahto, G. and M.B. Kumar, Health Education & Wellness, Yoga Education, Sports, Nutrition & Fitness. 2023: Shashwat Publication.